Observing efficient systematic collaboration through a C-section experience
My C-section went so smoothly not because any particular stage was amazing, but because the whole system worked well together.
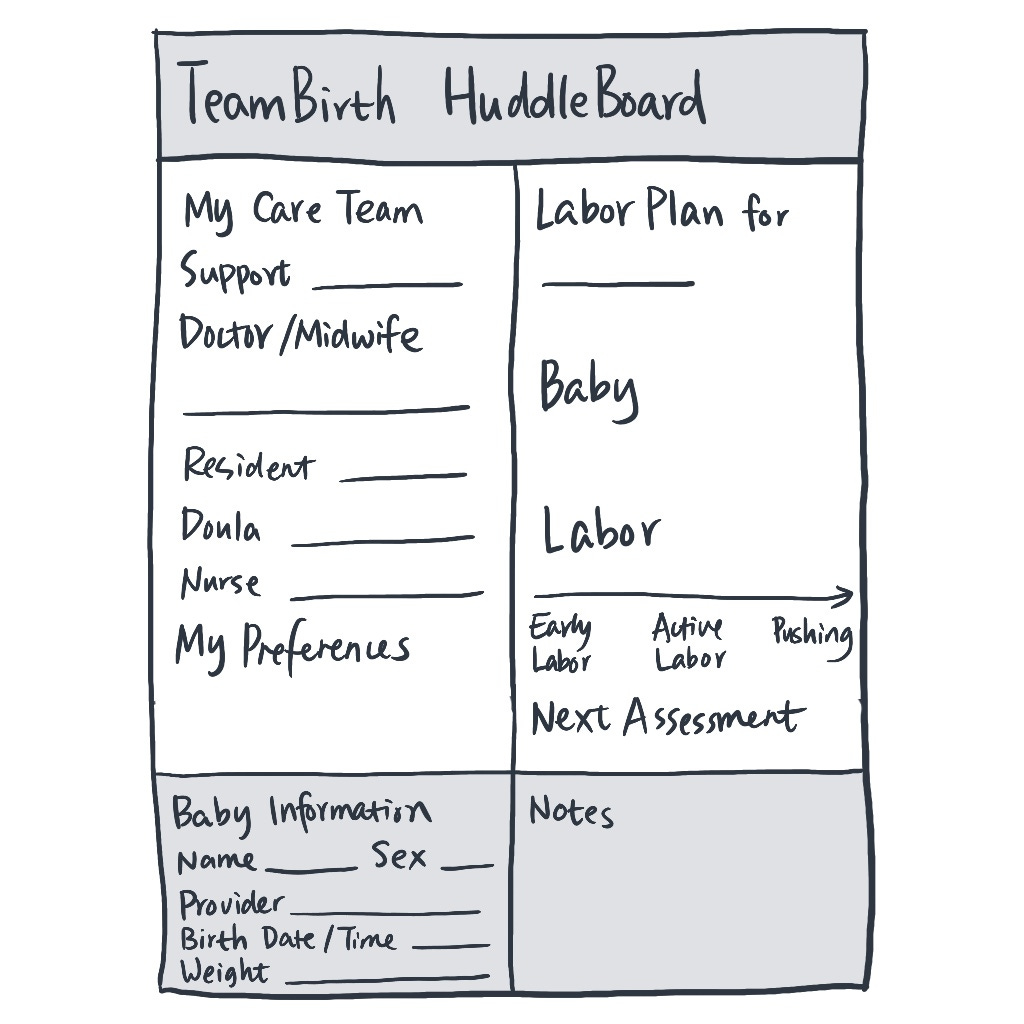
I had to stay in the hospital for a couple of days because of my C-section procedure. On the morning of surgery, I was sitting in bed getting fetal heart monitoring when I noticed a whiteboard across from me. At the top, it said “Huddle Board,” and below that it clearly listed my name, my husband’s name, the attending doctor, and other information.
Seeing the word “Huddle” made me smile—that’s what we call our team meetups when we’re developing software!
Looking back now, this whole C-section process showed me how an efficient system works, with my surgery being like one project running inside this bigger system.
How the system works
My surgery went really well, and my recovery has been smooth so far. If I think of this surgery as a project, it worked so well because this hospital has built a well-trained, efficient system. Each medical person plays different roles in this system—nurses might handle several rooms at once, midwives have other jobs during regular hours, anesthesiologists work with different departments, but when there’s a C-section surgery, they all smoothly switch into their specific roles for this project.
It’s just like an efficient software development system. Tasks move from planning to design to development to testing, and each stage has someone clearly in charge. My C-section procedure worked the same way: from getting ready for surgery to the actual operation to recovery afterward, each stage had different people in charge who worked efficiently together.
Stage one: Getting ready for surgery
The main people in this stage were scheduling staff, obstetricians, and nurses. Someone called me to set up meetings with the obstetrician about different delivery options; someone sent me detailed preparation instructions, explaining exactly how to clean and sterilize before surgery; someone else scheduled the surgery time.
On surgery day, I showed up at the scheduled time and immediately had a nurse come greet me—she was my main contact person for this stage. She took me to a room that was already set up and started monitoring my baby’s heartbeat and checking my condition. This room was just for pre-surgery prep and watching patients for two hours after surgery; recovery happened in a different room. The division of work was really clear.
That Huddle Board really caught my attention. As a patient lying in bed, all the information I needed right away was written clearly where I could see it easily.
Stage two: The surgery
The surgical team included the obstetrician, anesthesiologist, nurses, and a midwife. Before surgery, each of these key people came to talk with me one-on-one, switching from their other jobs in the system to focus on my “project.” The anesthesiologist was especially thorough since we were meeting for the first time. He carefully explained what would happen and what risks were involved. I’ve noticed that healthcare in America works this way: they clearly explain the pros, cons, risks, and chances of different options, but the final decision is mine, as the patient.
During surgery, I was awake the whole time and could hear them talking to each other. The anesthesiologist kept calling out updates about my condition, and nurses gave real-time feedback on different measurements, making sure I stayed stable throughout. I really liked this open communication.
Stage three: Recovery
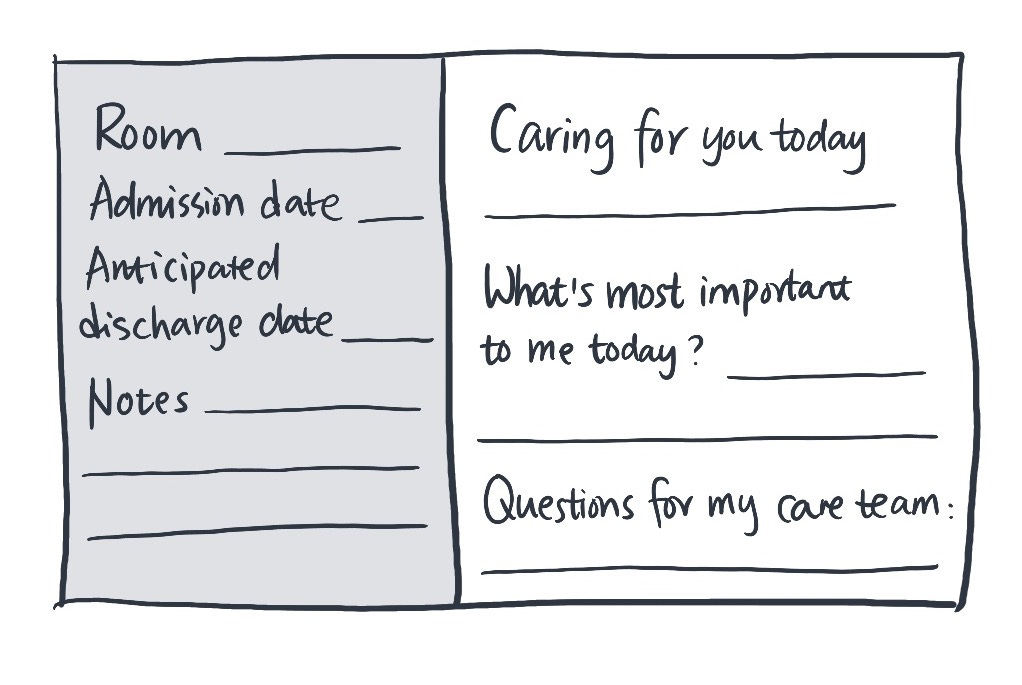
After surgery, they moved me to a postpartum room, which had two whiteboards. The side of the bed still had a large Huddle Board clearly showing basic information about me, my husband, and baby. Right across from my bed was another whiteboard where I could see immediate information: my current nurse’s name and important check-up and medication schedules. Since I needed to take several pain medications at different times, the nurse would write down medication names and timing, so I could easily keep track.
The main people in charge of this stage were postpartum nurses, who checked on me regularly and took care of both me and my newborn. The room also had necessary equipment, such as blood pressure monitors, pulse oximeters, and computers, so nurses could check my condition and record everything directly in the software system.
As someone receiving care from this system, I found the whole postpartum experience very thoughtful. Most of the time, I needed to stay in bed because I couldn’t move around much. For things like changing the baby’s diaper, I could use the call button on the bed to ask for nurse help; I could also order and eat meals right from bed, which was really convenient.
Before I left, a nurse did a detailed check, including making sure we were using the newborn’s car seat correctly. She gave me thorough instructions for taking care of the baby and my own recovery. More importantly, she clearly explained what situations would mean I needed to call a doctor or go to the emergency room, and all follow-up appointments were already scheduled. This meant for several weeks after going home, I didn’t need to worry about organizing these things.
Smooth handoffs between staff
During my hospital stay, because nurses work in shifts, I worked with over ten different nurses. What was amazing was how smoothly I communicated with each one.
I noticed that nurses did standardized verbal handoffs. While I didn’t see this process directly, several nurses told me things like “the previous nurse told me your situation is…” which showed that verbal handoffs are a really important part of this system.
Besides verbal handoffs, electronic records are also key to how efficiently the system works. This information isn’t just in the hospital’s internal system, I could also see each nurse’s notes about me through the hospital app on my phone. I really liked this transparency.
Tools that support the system
Besides these professional and efficient medical staff, the physical equipment and software tools are also important foundations that support how the whole system works. For equipment, each room had blood pressure monitors and pulse oximeters ready to use, so nurses didn’t need to bring them each time; for software, each room also had computers where staff could log in with their IDs and record patient information directly.
The software they use is made by a company called Epic Systems, which built electronic medical information systems for hospital staff and matching websites and mobile apps for patients. Epic’s system isn’t just for recording—it supports information flow throughout the whole medical system, letting each project (patient) move efficiently through the system. In this system, nurses’ notes get stored in a database that I as a patient can also access through my account. Some information, like medical history and vaccination records, also gets shared with other medical institutions, making it easy for connected facilities to reference when analyzing patient conditions later.
Thoughts on generative AI applications
With generative artificial intelligence making big changes across industries, I’ve been wondering where it might be useful in complex medical systems like this.
AI applications in these systems could work in different ways: some might only affect specific processes, while others might impact how the whole system operates. But I think when considering AI applications, we need to think systematically, looking not just at direct improvements but also considering possible effects on other processes. For example, how to help systems better predict and allocate resources, or how to make information flow more smoothly between different stages. This could include giving analysis and alerts to doctors and nurses based on patient conditions, or helping with backend staff scheduling when monitoring data shows problems. While I was in my room, the nurse taking care of me had to quickly check on me and then rush off because another patient had high blood pressure. If AI could analyze the overall situation ahead of time and help coordinate staffing, the whole system might work even better.
However, in healthcare, any automation has to be completely accurate. I’ve had automated systems get my baby’s vaccination appointment times wrong, and I had to call to fix it—this kind of mistake is totally unacceptable in medical systems.
What this taught me about systematic thinking
My C-section went so smoothly not because any particular stage was amazing, but because the whole system worked well together. Everyone was professional and efficient, knowing exactly what to do and when, and understanding how to work with others throughout the system.
This experience really showed me the power of an efficient system. As a user experience designer, I need to remember that any design is part of a bigger system, requiring me to think about what comes before and after it and how it works with the whole setup. This reminds me to think from a higher level when designing, making sure users have good experiences at every point in their journey.